
Just like most diabetics, I have checked my blood glucose levels twice in a short period of time out of curiosity to find that my glucose meter gives different readings. At first I thought I may have had a faulty meter, but for me and my personal needs a 10% margin of error is not a big deal. Since then I have learned a lot about how different meters work, improvements in the technology used in home testing supplies, government controlled standards for accuracy and the general needs of different kinds of diabetic patients through my work and community engagement.
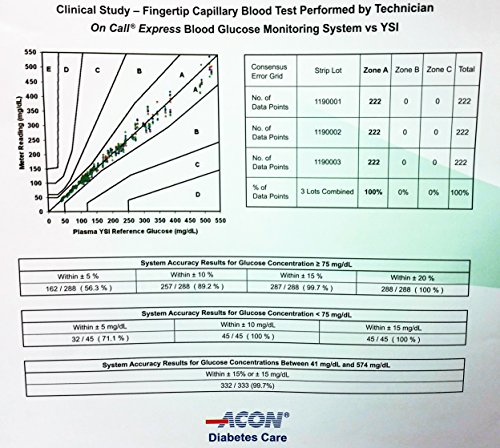
The short answer regarding meter accuracy is that the technology currently used in home diabetes testing supplies are only capable of testing within a 10-20% +/- margin of error. The FDA mandates minimum accuracy standards for testing supplies in the US, currently following the ISO 15197:2013 standard of 95% of tests must be within +/- 20% for results above 75 mg/dl and +/-15% for results below 75 mg/dl. This standard was issued in 2013, and the majority of manufacturers have redesigned their meters for better accuracy, increased consistency and ease of use since then.
Even though a 15% margin of error might seem large on the surface, Robert Ratner, MD, FACP, the American Diabetes Association’s chief scientific and medical officer says “[This level of] accuracy is sufficient for reliable clinical decision making and therapy”. In most cases results taken from an at home blood glucose meter would suggest similar treatment decisions as a result someone would get using laboratory equipment.
How Does a Glucose Meter Work?
To understand why a meter could give differing readings, you first have to understand how they work. The testing strip contains an enzyme that interacts with the glucose in your blood. The mixture generates electrons, which are then converted to an electrical current. The current is transferred from the strip to the meter, which is programmed to read the electrical current as the final numeric value.
The variables involved from the manufacture of the enzyme to the actual testing procedure and the test subject are immense. In earlier generations meters had to be coded, or the manufacturer sent a coding chip with each box of strips to alter the formula to match the slight variations in each batch of strips. Today most strips are coded so the end user is unaware that their meter is calibrating itself to each new batch of strips used.
Hospital labs achieve a higher degree of accuracy by controlling variables more closely. Their equipment is kept in an environment with consistent temperature and humidity, and is programmed for those variables. Nurses and technicians are professionally trained to limit variations in testing. The equipment is built with more costly, and more consistent components. Most importantly, blood samples are separated and only the blood plasma is tested (all home testing kits test whole blood). Finally, laboratory machines test a much larger sample for over a minute; at home testing devices are designed to use the smallest sample possible and deliver the fastest results. Even with all those differences laboratory tests generally still have a +/-4% margin of error. Some lab equipment exhibits a +/-5% to +/-8% margin of error.
The most important thing about blood glucose meter accuracy is that you can use the results to make competent and confident decisions regarding your care. If you feel like your meter is inaccurate enough to cause problems with your dosing or treatment, take it with you during your next doctor visit and test simultaneously with the blood sample being drawn for lab testing (be sure to find out if your meter results are converted to Plasma levels or if they’re being reported as whole blood levels). If your reading would have specified a noticeable difference in your treatment, it might be something to worry about. Millions of people use home testing glucose meters every year however, and the FDA receives between 25,000 and 30,000 reports about malfunctions and user errors relating to glucose meters annually. Their standards take real world scenarios and the data associated with those reports into consideration.
Why is Your Diabetes Meter Inaccurate?
Starting with the strip, the chemical process involved relies on an exact amount of blood entering the reservoir in a prescribed amount of time, at a pre-determined temperature and an educated guess assigned to the composition of the blood itself. Not only will one person’s blood differ from another’s in chemical makeup and red blood cell count, contagions on your skin AND the presence of water or alcohol after cleaning can affect the results.
For the strip to have a chance at giving a perfect result you need to use the same amount of blood and fill the strip in the same time frame every time; your blood and the enzyme in the strip needs to be at consistent temperatures. If you think that using two drops of blood from the same lancing site should be more accurate, you’d actually be wrong. The first drop of blood will have more extracellular fluid content than proceeding drops.
Known Variables to Interfere with Test results
- Meter not calibrated regularly
- Storage and handling of test strips
- Not properly cleansing the test site
- Testing site damp from alcohol prep or water
- Not enough blood applied to test strip
- Altitude, temperature, and humidity
- Change of Test Site
- Inconsistent Red Blood Cell levels due to dehydration, anemia or polycythemia
- Interfering substances (Vitamin C, acetaminophen, and uric acid)
Diabetic testing supplies are by design not extremely accurate, but quality control during manufacturing and transport can further affect accuracy. Proper storage by the retailer and finally the patient in a climate controlled environment and keeping an eye on the expiration date will help you limit additional inconsistencies.
4 Tips to Maximize The Accuracy of Your Glucose Meter
Properly Store and Handle Strips– There are two components on your strips that are very sensitive, the chemical that reacts with your blood and the conductor that transmits the reading to your meter.
- Keep your strips away from sunlight and moisture
- Testing has shown that cooler temperatures help keep the strips longer
- Make sure to seal your vial after you take a strip out
- Avoid getting the oil on your fingers on the chip/ connection point, it can affect the electrical current
Wash your hands– Try to limit contamination by washing your hands, and drying them thoroughly before testing. I would recommend waiting five minutes afterward and then testing to give your hands a chance to dry completely.
Be consistent– Try and use the same amount of blood and get the blood from the same part of your finger. Aim to get as many tests in the same room of your home at the same times of day ( this will control temperature and also make your benchmarks and trends more meaningful). Only use results from the same meter for intense comparison.
Repeat your tests– When an engineer requires a greater degree of accuracy than their equipment is capable, they will often repeat the test a number of times and use the average. This will also allow you to identify outliers or faulty strips.
Some Things to Consider Regarding Glucose Meter Accuracy
For most readings the current accuracy standards are more than acceptable for making treatment decisions – the guidelines require a higher degree of accuracy in the range where a smaller deviation in treatment could lead to serious consequences. Some patients will also be more susceptible to treatment variations due to inaccuracy, particularly children or adults with a lower body weight. If you are concerned with your meter’s accuracy, I would recommend running a test scenario for various levels of tolerance to find out what levels of inaccuracy your treatment can withstand. It’s important to understand the relationship between your test results and your self administered treatment.
Even though manufacturers have been successful at introducing incrementally better products, it will take a holistic re design and breakthrough to make a substantial increase in accuracy. While some meters are slightly more accurate in testing (The Accu-Chek and FreeStyle meters consistently maintain high accuracy scores in testing), we ultimately decided that the On Call Express meter offered the best return on investment, with comparable accuracy testing results of even the highest rated meters – and better results than some of the most popular (and most expensive) alternatives at a substantial savings.
According to the test results we accumulated from manufacturers and 3rd parties prior to selecting the meters we would sell; At the lower threshold where accuracy is most important, only 3 brands had meters that achieved 100% of results within a 10% margin, and those were Accu-Chek, FreeStyle and On Call Express. 71% of the On Call Express results were within 5% (As compared to the One Touch Verio Pro which only had 53% of tests within the 10% margin [Vs. 100% for the On Call Express], and only 21% within the 5% margin). Overall the relatively high accuracy and incredibly good value of the On Call Express won us over.





